This article has been written in partnership with Kelly McCabe, CEO and co-founder of Perci Health (opens a new window).
Cancer is one of the major drivers for health cost trends in terms of cost and increasingly incidence. Businesses offering health and risk benefits increasingly need to understand and address the hidden costs beyond insurance claims.
Statistics suggest that one in two people in the UK will be diagnosed (opens a new window) with cancer in their lifetime and currently over three million people in the UK are living with cancer, with this figure set to increase to £5m by 2030. Of those affected, 36% are of working age (opens a new window).
The good news is that due to rapid progress in the screening, diagnosis and management of cancer survival rates are rising. Figures from Cancer Research UK show that 50% of people diagnosed with cancer live more than 10 years beyond their diagnosis (opens a new window).
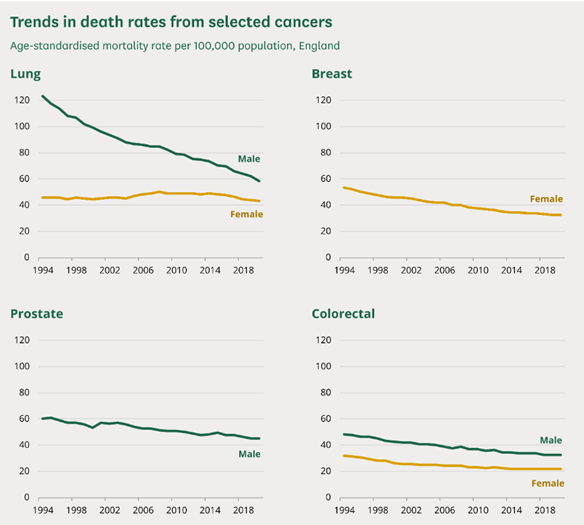
Source: House of Commons Library, ONS NOMIS, Mortality statistics (opens a new window)
While survival rates are rising, the cost and duration of cancer therapy is significantly increasing as expensive but effective novel therapies are introduced. One person’s treatment can severely impact a whole group’s insurance premiums, meaning insurers (and employers) need to constantly monitor and review the cancer cover they provide in the future, within the insurance policy itself and beyond into areas such as prevention and broader support.
Direct and indirect costs of cancer
The economic burden of cancer doesn’t consist only of treatment costs as it has two components – direct and indirect costs:
Direct costs include all the resources necessary for prevention, treatment, and cancer care
Indirect costs include resources lost due to inability to work – for both those with a cancer diagnosis and the increasing number of people caring for a loved one with cancer
Cancer Costs (opens a new window), a study conducted by independent, educational charity Demos, suggested that the indirect costs of cancer to the UK economy from lost wages and benefits to be at least £7.6 billion a year.
Returning to work after cancer treatment has historically provided many living with, and beyond cancer, a sense of stability and normality that they crave, as well as much needed financial support.
Through more effective treatment and management of the condition, those affected are able to return to the workforce earlier, benefiting not only the patient but also their family and society overall.
A gap in cancer treatment and support
Beyond diagnosis and treatment there is a gap in service provision with cancer patients describing a sense of ‘abandonment’ once their treatment ends. This suggests the existence of an increasing urgency for accessible, effective, long-term support for people with cancer (beyond the routine hospital care) driven by scientific advancements in cancer treatment plus the changing expectations of consumers.
A recent systematic review (opens a new window) concluded that fear of cancer progression, treatment disruption, as well as fear of Covid-19 infection and isolation, have led to increased levels of psychological distress, anxiety and depression among cancer patients globally over the past two years.
Presently there is little-to-no support focusing on helping employees to remain in or return to work, even for those with comprehensive medical insurance. This is despite predictions that a greater proportion of the workforce will be impacted by cancer in the future.
Well-coordinated, multi-modal therapy (delivered by nurses, physiotherapists, dietitians, and other cancer specialists) is the gold standard; proven to accelerate return to work and prevent long-term complications. Reducing the impact of cancer on employees and their families requires a wide range of cancer support services focused on rehabilitation and recovery from a physical, psychological, and social perspective.
If these services are provided virtually, geographical barriers are dissolved and in turn, employees can reduce the time off needed to attend appointments. There are many validated tools to capture quality of life and symptom-specific data being used within the clinical setting that can now be applied to longer-term follow-up, including in the workplace. These can help monitor and support those impacted by cancer.
The role of the employer
Employers have started to put pressure on providers of cancer support (and other chronic conditions) via employee benefits programmes to be accountable for their clinical outcomes, as opposed to simply focusing on engagement or utilisation.
Businesses can take a number of steps to support employees with cancer, as well as cancer carers, in returning to the workplace. How well the physical, psychological, and social wellbeing needs of cancer patients are met, can determine whether their transition back to work will be successful or not.
Speak with employees impacted by cancer to understand what their needs are to return to the workplace confidently from both a physical and mental perspective.
Have a clear understanding of the treatments and support offered from across your employee benefits programme including private medical, group income protection and employee assistance programme, both during primary cancer treatment as well as after. This will help to identify any potential gaps in care provision.
Consider taking an active, innovative role in improving access for employees to crucial cancer support services by partnering with or signposting to expert providers in this area.
Lockton is running a webinar with Perci Health on 2 February 2023 as part of World Cancer Day on ‘The true cost of cancer in the workplace’. Regsiter now (opens a new window).

For more information on health support in your business and services available, including Perci health, please contact:
Chris Rofe, Partner
Lockton People Solutions
T: +44 (0) 79 3030 7266
E: chris.rofe@lockton.com (opens a new window)
Kelly McCabe, CEO
Co-founder of Perci Health, the world's first online platform giving access to multidisciplinary cancer teams focused on recovery from a physical, psychological, and practical point of view. A registered oncology dietitian with first-hand experience of working with hundreds of cancer patients, and senior management experience within both the NHS and private healthcare.
